Reports
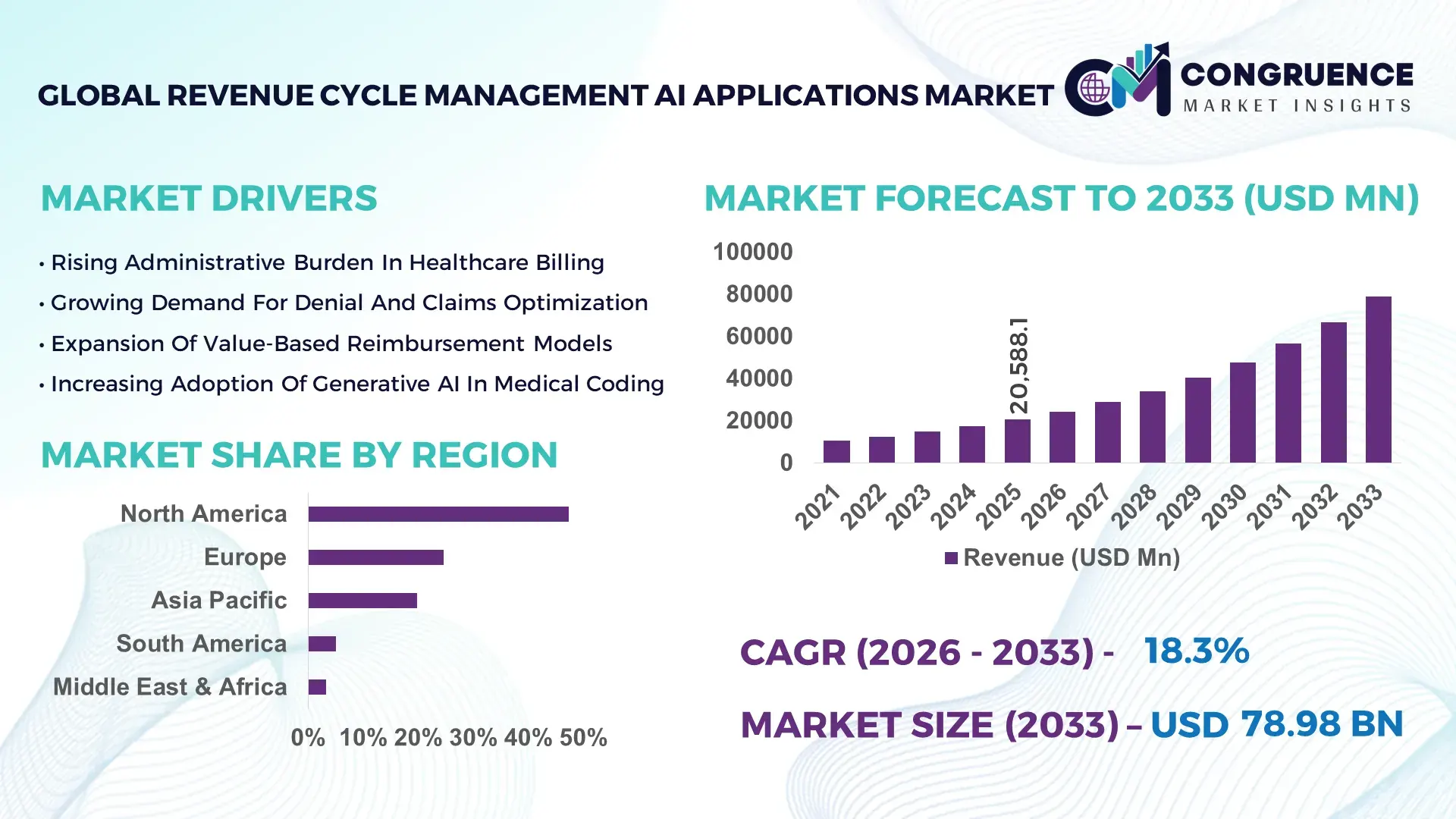
The Global Revenue Cycle Management AI Applications Market was valued at USD 20,588.1 Million in 2025 and is anticipated to reach a value of USD 78,975.8 Million by 2033 expanding at a CAGR of 18.3% between 2026 and 2033, according to an analysis by Congruence Market Insights. Growth is fueled by accelerating digital transformation in healthcare finance operations and increasing pressure to reduce claim denials and administrative costs.
The United States represents the most advanced Revenue Cycle Management AI Applications market globally, supported by over 6,100 hospitals and more than 33 million annual inpatient admissions integrated into digital billing ecosystems. In 2025, more than 72% of large healthcare systems deployed AI-enabled claims scrubbing, coding automation, or denial prediction tools. Annual investment in healthcare IT modernization exceeded USD 18 billion, with a significant portion allocated to AI-driven revenue optimization platforms. Automated prior authorization systems reduced manual processing volumes by 34%, while AI-assisted medical coding improved accuracy levels to above 95% across leading hospital networks. Specialty clinics and multi-state provider groups increasingly deploy predictive analytics engines to manage reimbursement risk, reflecting advanced operational maturity.
Market Size & Growth: Valued at USD 20,588.1 million in 2025, projected to reach USD 78,975.8 million by 2033 at 18.3% CAGR, driven by automation of claims and reimbursement workflows.
Top Growth Drivers: AI-based denial reduction (45%), coding automation efficiency (38%), predictive revenue analytics adoption (33%).
Short-Term Forecast: By 2028, intelligent claims management systems are expected to reduce denial rates by 28%.
Emerging Technologies: Generative AI for medical coding, machine learning-based denial prediction, robotic process automation in billing.
Regional Leaders: North America projected at USD 36.4 billion by 2033; Europe at USD 18.2 billion driven by public health digitization; Asia-Pacific at USD 16.7 billion supported by private hospital expansion.
Consumer/End-User Trends: Over 59% of large provider networks prioritize AI dashboards for real-time revenue visibility.
Pilot or Case Example: In 2024, a hospital group achieved 22% faster reimbursement cycles through AI-based eligibility verification.
Competitive Landscape: Epic Systems leads with ~24% enterprise integration presence, followed by Oracle Health, R1 RCM, Optum, and Change Healthcare.
Regulatory & ESG Impact: Value-based care mandates driving outcome-linked billing optimization tools.
Investment & Funding Patterns: More than USD 4.2 billion invested globally in healthcare AI revenue platforms between 2023–2025.
Innovation & Future Outlook: Real-time payer-provider interoperability and predictive cash-flow modeling shaping next-gen systems.
Hospitals contribute approximately 54% of AI-enabled revenue cycle deployments, physician groups 26%, and ambulatory surgical centers 12%, while diagnostic labs and specialty clinics account for 8%. Innovations in AI-powered denial analytics, automated coding engines, and intelligent patient billing portals are improving collection rates and compliance accuracy. Regional growth is strongest in North America and Asia-Pacific, where healthcare digitization initiatives and private hospital investments are accelerating adoption of Revenue Cycle Management AI Applications.
The Revenue Cycle Management AI Applications Market has become strategically critical for healthcare providers seeking financial resilience amid rising reimbursement complexity and staffing shortages. AI-powered predictive denial analytics delivers 30% improvement compared to traditional rule-based claims review systems, significantly enhancing first-pass claim acceptance rates.
North America dominates in transaction volume, while Asia-Pacific leads in new digital platform adoption with over 61% of private hospital chains implementing AI-integrated billing solutions. By 2027, generative AI-based coding assistants are expected to improve coding productivity by 25%, reducing backlogs and accelerating revenue realization.
Compliance and ESG priorities are increasingly shaping procurement strategies. Healthcare organizations are committing to 40% reduction in paper-based billing statements by 2030, aligning with sustainability goals and digital engagement strategies. In 2024, a multi-state U.S. provider network achieved a 19% reduction in average accounts receivable days through AI-driven workflow automation.
Future pathways emphasize interoperability with electronic health records, payer systems, and telehealth platforms. Predictive cash-flow modeling, automated prior authorization, and real-time eligibility verification will define competitive differentiation. As regulatory oversight intensifies and reimbursement models shift toward value-based care, the Revenue Cycle Management AI Applications Market is emerging as a foundational pillar of operational efficiency, compliance assurance, and sustainable financial growth across global healthcare ecosystems.
The Revenue Cycle Management AI Applications market is shaped by increasing healthcare digitization, reimbursement policy shifts, and rising administrative cost pressures. Growing claim denial rates, which exceed 10% in many healthcare systems, drive adoption of predictive analytics and automated claims scrubbing solutions. Integration with electronic health record platforms enhances data-driven decision-making and operational transparency. Hospitals and provider networks are prioritizing automation to offset workforce shortages, with AI-assisted coding reducing manual workload by up to 35%. Regulatory mandates supporting value-based reimbursement further accelerate demand for advanced analytics. Competitive intensity is increasing as established healthcare IT vendors and AI-native startups expand platform capabilities, reinforcing innovation cycles and technology convergence.
Claim denials and reimbursement delays significantly impact healthcare cash flow, with denial rates exceeding 12% across large hospital networks. AI-driven denial prediction models analyze thousands of claim variables, improving first-pass approval rates by 20%–30%. Automated eligibility verification reduces registration errors by 26%. As payer rules grow increasingly complex, healthcare organizations are prioritizing AI-based workflow automation to maintain financial stability. These measurable improvements in operational efficiency and revenue capture are driving broader adoption of Revenue Cycle Management AI Applications.
Integration with legacy hospital information systems remains challenging, with implementation timelines averaging 6–12 months. Data interoperability gaps can increase deployment costs by 18%. Additionally, healthcare data privacy regulations require robust encryption and compliance audits, elevating IT expenditures. Smaller clinics often lack the infrastructure needed for seamless AI integration. These structural barriers can slow adoption, particularly in resource-constrained healthcare environments.
Value-based reimbursement models reward outcomes rather than service volume, increasing the need for predictive analytics and cost modeling. Over 55% of U.S. healthcare payments are now tied to value-based structures, requiring advanced revenue forecasting tools. AI-driven risk adjustment analytics improve reimbursement accuracy by 24%. Expanding telehealth services also create opportunities for automated billing and real-time payer validation, broadening platform application scope.
Frequent updates to payer reimbursement policies require continuous algorithm refinement. Healthcare providers must adjust coding standards and billing workflows regularly, increasing system maintenance demands. Regulatory audits and compliance checks add administrative layers, potentially extending claim resolution timelines. Maintaining algorithm transparency and audit readiness remains a persistent operational challenge.
Adoption of Generative AI for Coding Automation: In 2025, 46% of large hospital systems integrated generative AI tools for medical coding, improving coder productivity by 27% and reducing documentation backlogs by 22%.
Real-Time Denial Prediction Analytics: AI-powered predictive engines reduced claim denial rates by up to 28%, with over 60% of enterprise providers deploying machine learning dashboards for reimbursement forecasting.
Expansion of Robotic Process Automation in Billing: Approximately 52% of mid-to-large healthcare organizations adopted robotic billing automation, decreasing manual task volumes by 35% and accelerating payment posting accuracy by 18%.
Digital Patient Engagement and Payment Portals: AI-enabled patient billing portals increased digital payment adoption to 64%, reducing average collection cycle time by 16% across multi-specialty provider networks.
The Revenue Cycle Management AI Applications market is segmented by type, application, and end-user structure. Solutions range from AI-driven coding automation and denial management platforms to predictive revenue analytics and eligibility verification systems. Applications span claims processing, billing optimization, prior authorization management, and cash-flow forecasting. End-users include hospitals, physician groups, ambulatory surgical centers, and diagnostic laboratories. Market segmentation reflects differences in claim volumes, reimbursement complexity, and digital maturity levels. Large healthcare systems prioritize enterprise-scale analytics, while smaller clinics adopt modular AI billing solutions tailored to limited IT infrastructure.
Denial management AI platforms account for approximately 41% of adoption, driven by their ability to reduce claim rejection rates and improve cash flow predictability. Medical coding automation systems represent 29%, while predictive revenue analytics tools hold 18%. However, generative AI coding assistants are the fastest growing segment, projected at 21.5% CAGR due to increasing documentation complexity. The remaining 12% includes eligibility verification and payment posting automation tools.
In 2025, a national health IT authority reported that AI-based coding systems achieved over 95% coding accuracy across participating hospital networks.
Claims processing optimization holds 44% share, reflecting the centrality of reimbursement workflows. Billing automation accounts for 26%, while denial prediction and appeals management contribute 19%. Predictive financial analytics is expanding fastest at 19.2% CAGR, supported by value-based care reimbursement models. In 2025, more than 38% of enterprises globally reported piloting Revenue Cycle Management AI Applications for customer experience platforms within healthcare systems.
In 2025, a public health agency highlighted that AI-assisted billing systems reduced average reimbursement cycles by 20% across 150 hospitals.
Hospitals represent 54% of total adoption, given high claim volumes and reimbursement complexity. Physician groups account for 26%, while ambulatory surgical centers and diagnostic labs collectively hold 20%. Ambulatory centers are the fastest-growing end-user segment, projected at 20.1% CAGR due to outpatient procedure expansion. In 2025, 42% of hospitals in the US reported testing AI models combining clinical documentation with billing data to optimize reimbursement accuracy.
In 2025, a national healthcare digitization program indicated that AI adoption among mid-sized clinics increased by 23%, enabling over 400 facilities to enhance revenue tracking and denial prevention systems.
North America accounted for the largest market share at 47.3% in 2025 however, Asia-Pacific is expected to register the fastest growth, expanding at a CAGR of 20.1% between 2026 and 2033.

North America processed more than 4.8 billion healthcare claims annually through AI-enabled Revenue Cycle Management platforms, with over 72% of large hospital systems deploying predictive denial analytics. Europe held 24.6% share, driven by national health digitization programs across Germany, the UK, and France. Asia-Pacific accounted for 19.8%, with private hospital chains in India and China increasing AI billing automation adoption by over 35% year-over-year. South America and Middle East & Africa collectively represented 8.3%, supported by expanding private healthcare networks and digital claims modernization initiatives exceeding USD 1.2 billion in combined regional healthcare IT investments.
How is advanced healthcare digitization transforming intelligent revenue optimization systems?
This region represents approximately 47.3% of the Revenue Cycle Management AI Applications market in 2025, with more than 4,000 hospital networks and 200,000 physician practices utilizing AI-driven billing solutions. Key demand originates from hospitals, ambulatory surgical centers, and multi-state healthcare systems facing claim denial rates exceeding 12%. Regulatory reforms promoting price transparency and value-based reimbursement have accelerated AI analytics deployment. Over 65% of large providers integrated machine learning-powered denial prediction tools, reducing accounts receivable days by up to 19%. A leading domestic healthcare IT vendor expanded generative AI coding modules, improving coding accuracy to above 96%. Regional enterprise behavior reflects high digital maturity, with strong integration across electronic health records and payer systems.
Why are compliance-driven healthcare reforms accelerating AI billing modernization?
Europe accounted for nearly 24.6% of the Revenue Cycle Management AI Applications market in 2025, led by Germany, the UK, and France, which together represent over 60% of regional AI-enabled claims processing volumes. Public healthcare digitization initiatives increased AI adoption across 1,800 hospitals. Regulatory frameworks emphasize data protection, audit transparency, and standardized reimbursement coding. Approximately 54% of large public hospitals adopted predictive analytics for reimbursement optimization. A regional healthcare IT firm implemented AI-based eligibility verification systems, improving claim approval rates by 17%. Consumer behavior is influenced by regulatory oversight, driving demand for explainable AI models and secure billing automation platforms.
What drives rapid expansion of AI-powered claims automation across emerging healthcare ecosystems?
Asia-Pacific ranks as the fastest-growing region, with over 2,300 private hospitals integrating AI-enabled revenue optimization tools in 2025. China, India, and Japan account for more than 73% of regional digital billing deployments. Healthcare infrastructure investments exceeding USD 10 billion annually are accelerating AI platform integration. Real-time eligibility verification systems reduced manual billing errors by 28% across major metropolitan hospital chains. A regional AI software provider introduced cloud-based denial analytics platforms serving over 500 healthcare facilities. Adoption is strongly supported by mobile-first healthcare administration systems and growing outpatient procedure volumes.
How are healthcare modernization programs improving financial workflow efficiency?
South America represents 5.1% of the Revenue Cycle Management AI Applications market, led by Brazil and Argentina. Private hospital expansion increased digital claims automation by 21% in 2025. Government incentives supporting health IT upgrades facilitated AI deployment in more than 350 mid-sized healthcare facilities. Automated payment reconciliation improved reimbursement cycle efficiency by 14%. A regional health analytics company implemented AI-based billing dashboards across public-private hospital partnerships, enhancing revenue visibility. Healthcare providers prioritize cost-efficient automation tools to manage rising administrative workloads.
Why is digital health transformation strengthening intelligent billing adoption?
Middle East & Africa accounts for 3.2% of the global Revenue Cycle Management AI Applications market in 2025, with UAE and South Africa leading adoption. Smart hospital programs increased AI billing system deployment across 220 facilities. Regional healthcare IT spending surpassed USD 2.5 billion, with significant allocation to AI-driven claims management. Automated prior authorization reduced approval turnaround time by 18%. A regional healthcare technology integrator deployed AI revenue analytics platforms across specialty clinics, improving financial reporting accuracy. Demand is primarily concentrated in private hospital networks and urban healthcare centers.
United States Revenue Cycle Management AI Applications Market – 44.1%: Extensive hospital network digitization and high claim volumes support large-scale AI billing integration.
Germany Revenue Cycle Management AI Applications Market – 9.8%: Strong public healthcare modernization and regulatory-driven billing standardization accelerate AI deployment.
The Revenue Cycle Management AI Applications market demonstrates a moderately consolidated competitive structure, with approximately 60 active global vendors delivering AI-driven billing, coding, and denial management platforms. The top five players collectively account for nearly 58% of enterprise-scale deployments, reflecting strong brand recognition and integration capabilities. Competitive differentiation focuses on algorithm accuracy, interoperability with electronic health records, and real-time payer connectivity. In 2025, over 40 strategic partnerships were formed between healthcare providers and AI platform vendors to enhance predictive revenue analytics. Product development cycles average 12–18 months, with 62% of vendors incorporating generative AI coding modules. Innovation intensity is high, as vendors compete on measurable outcomes such as 20%–30% reduction in denial rates and 15% improvement in cash-flow forecasting precision. Market participants emphasize compliance-ready platforms and scalable cloud-native architectures to secure long-term contracts with large healthcare networks.
Optum Inc.
Change Healthcare
Cerner Corporation
McKesson Corporation
Athenahealth
Allscripts Healthcare Solutions
Experian Health
NextGen Healthcare
Conifer Health Solutions
Waystar
FinThrive
Technological advancements in the Revenue Cycle Management AI Applications market center on predictive analytics, generative AI automation, and robotic process orchestration. Modern AI platforms process over 10 million claim records daily, analyzing more than 500 billing variables to enhance approval accuracy. Machine learning denial prediction engines improve first-pass claim rates by up to 30%.
Generative AI-based coding assistants reduce documentation review time by 27%, supporting coder productivity amid workforce shortages. Robotic process automation handles repetitive billing tasks, cutting manual processing volumes by 35%. Real-time interoperability APIs integrate seamlessly with electronic health records and payer databases, reducing eligibility verification errors by 26%.
Advanced analytics dashboards provide financial visibility across multi-location healthcare networks, enabling 18% faster reimbursement tracking. Cloud-native deployment models allow scalable integration across hospital systems exceeding 500 beds. Data encryption standards meet stringent healthcare compliance requirements, safeguarding patient information across millions of transactions annually. Emerging technologies include predictive cash-flow modeling, automated prior authorization bots, and AI-driven patient payment optimization engines, reinforcing operational resilience and strategic financial intelligence across healthcare enterprises.
In February 2025, Oracle Health expanded its AI-powered revenue cycle management suite by integrating generative AI coding assistance into its electronic health record platform, enhancing automated documentation workflows and improving coding accuracy for hospital clients. Source: www.oracle.com
In October 2024, R1 RCM announced enhancements to its intelligent automation platform, deploying machine learning denial analytics across multiple health systems to improve first-pass claim rates and accelerate reimbursement cycles. Source: www.r1rcm.com
In May 2025, Epic Systems introduced advanced predictive analytics features within its revenue cycle modules, enabling real-time denial risk scoring and improved financial performance tracking for large provider networks. Source: www.epic.com
In August 2024, Waystar launched AI-driven eligibility verification and payment integrity tools designed to reduce claim errors and improve payment posting efficiency across ambulatory and hospital facilities. Source: www.waystar.com
The Revenue Cycle Management AI Applications Market Report delivers comprehensive analysis across AI-driven billing automation, denial management, predictive analytics, and coding optimization technologies. The scope covers hospital networks, physician practices, ambulatory surgical centers, and diagnostic laboratories, representing over 80% of healthcare claim processing volumes globally.
Geographic coverage spans North America, Europe, Asia-Pacific, South America, and Middle East & Africa, with detailed country-level evaluation of digital healthcare adoption trends. The report assesses more than 60 AI vendors, focusing on platform interoperability, algorithm accuracy, and compliance capabilities.
Applications analyzed include claims processing, prior authorization automation, revenue forecasting, payment posting, and patient engagement billing portals. Technological layers such as generative AI coding engines, robotic process automation bots, and predictive denial analytics models are evaluated based on deployment scalability and performance benchmarks.
Quantitative insights include claim volume processing capacity, denial rate reduction percentages, automation penetration rates, and digital payment adoption metrics. Emerging niche segments such as AI-powered value-based reimbursement analytics and cloud-native revenue optimization platforms are examined to provide strategic intelligence for healthcare executives, IT leaders, and financial decision-makers navigating the evolving Revenue Cycle Management AI Applications market.
| Report Attribute/Metric | Report Details |
|---|---|
|
Market Revenue in 2025 |
USD 20,588.1 Million |
|
Market Revenue in 2033 |
USD 78,975.8 Million |
|
CAGR (2026 - 2033) |
18.3% |
|
Base Year |
2025 |
|
Forecast Period |
2026 - 2033 |
|
Historic Period |
2021 - 2025 |
|
Segments Covered |
By Type
By Application
By End-User
|
|
Key Report Deliverable |
Revenue Forecast, Growth Trends, Market Dynamics, Segmental Overview, Regional and Country-wise Analysis, Competition Landscape |
|
Region Covered |
North America, Europe, Asia-Pacific, South America, Middle East, Africa |
|
Key Players Analyzed |
Epic Systems Corporation, Oracle Health, R1 RCM Inc., Optum Inc., Change Healthcare, Cerner Corporation, McKesson Corporation, Athenahealth, Allscripts Healthcare Solutions, Experian Health, NextGen Healthcare, Conifer Health Solutions, Waystar, FinThrive |
|
Customization & Pricing |
Available on Request (10% Customization is Free) |
